
Polymer science advances drug-delivery mechanisms to better break down cancerous tumors
The National Cancer Institute has indicated that in 2014, “it is estimated that there will be 1,665,540 new cases of all cancer sites and an estimated 585,720 people will die of this disease.”
That’s why Katie Bratlie, an assistant professor of materials science and engineering and chemical and biological engineering at Iowa State University, wants to create a more effective and efficient way to treat the disease. And so she is developing biodegradable polymers to improve chemoimmunotherapy—a type of chemotherapy that works with the immune cells to remove cancerous cells.
The immune cells she’s working with are white blood cells called macrophages. Found all across the human body, macrophages are considered the “first responders” to bodily injuries, removing bacteria and debris.
Despite being good for the rest of the body, macrophages in tumors make the prognosis for cancer patients much worse. That’s because these cells promote blood vessel growth, bringing nutrients to the tumor and helping it grow.
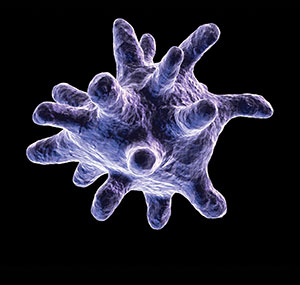
“Once those blood vessels are established, the tumor cells have a place to metastasize across the body,” explained Bratlie. Macrophages offer an advantage in that they take up drugs relatively easily, making them a great resource for Bratlie, who is determined to find a way to utilize the proprieties of tumor-associated macrophages for treating cancer.
She and her team are looking at a variety of chemical characteristic groups to uncover a functional group that will alter macrophage secretion profiles, essentially reprogramming the macrophage cells to act in a pro-inflammatory capacity, fighting off the tumor rather than promoting its growth.
When she finds the ideal polymer, she plans to integrate it into a hydrogel that will encapsulate a cancer-treating drug. Her technique would allow the medicine to be delivered directly to a growing tumor without impacting surrounding cells.
“Using this approach, the drugs used to treat a cancer will attach to a malignant cell and signal to macrophages and other white blood cells that the cancerous cells should be phagocytosed, or digested,” she explained.
As the team is analyzing cells and studying their responses to polymers in petri dishes in the lab, it is looking for apoptosis, or cell death, to ensure the treatment is effective in killing cancerous cells. The group is also conducting animal trials and collaborating with researchers who have expertise in animals and humans to explain tumors and physiology.
The ultimate dream, while likely many years down the road, is to bring the research to clinical trial. Bratlie says some day it may also be possible to personalize the macrophage response based on cancer stage and other factors, making for a more individualized approach to this combination cancer therapy.
Her research is also applicable in other areas, as macrophages are being studied across Iowa State’s campus, including their role in vaccines and parasitic diseases.
“Some diseases, like tuberculosis, actually reside inside the macrophage, so it doesn’t get destroyed. Instead it divides and stays. It’s a persistent infection,” she said. “If we could do something inside the microphage to remove the infection or attack it, that would be a great advancement.” Katie Bratlie (right), assistant professor of materials science and engineering and chemical and biological engineering, and Rachel Philiph, senior in materials science engineering and Goldwater Scholar, work together in Bratlie’s lab. White blood cells called macrophages are considered “first responders” to bodily injuries, removing bacteria and debris.